45 year old male with shortness of breath

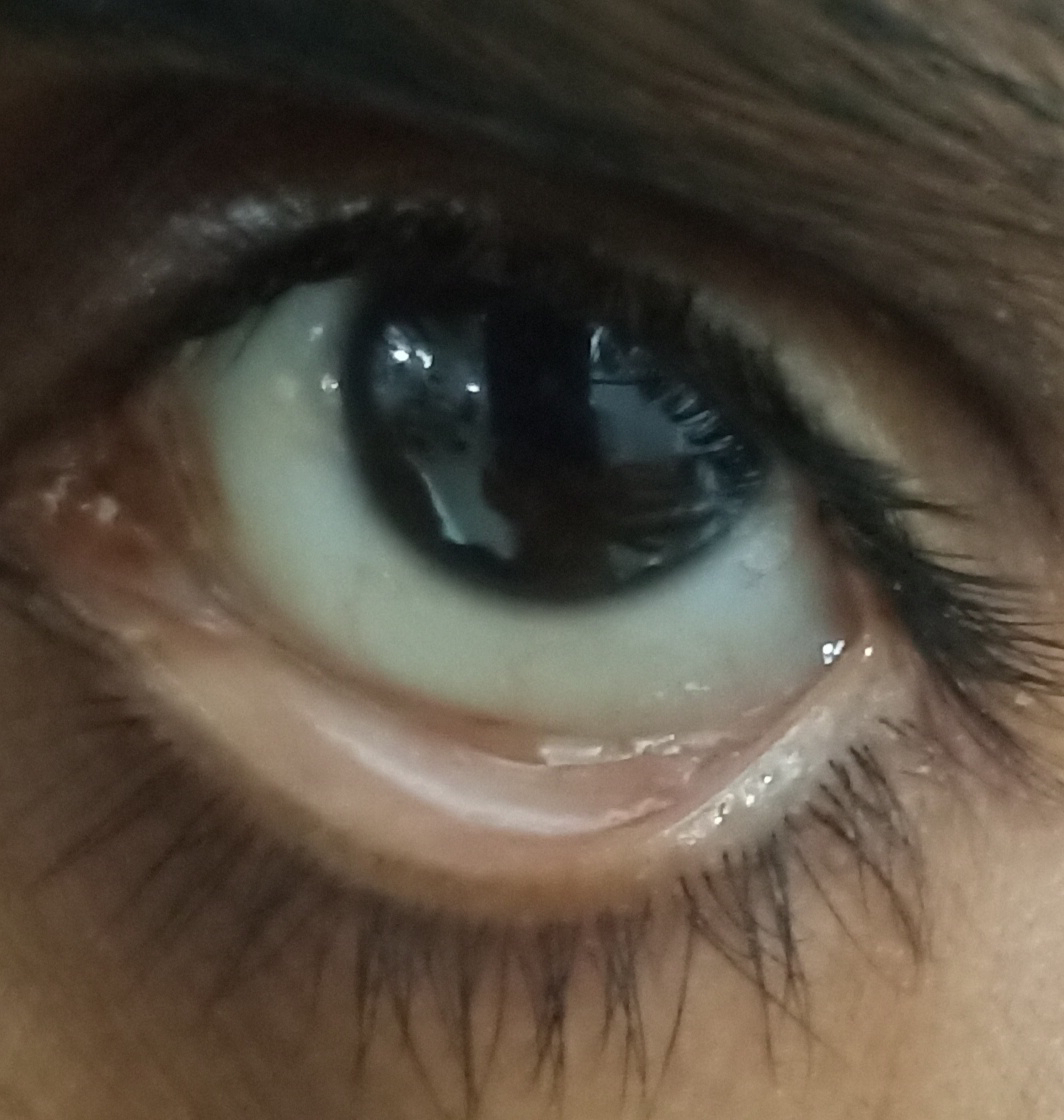
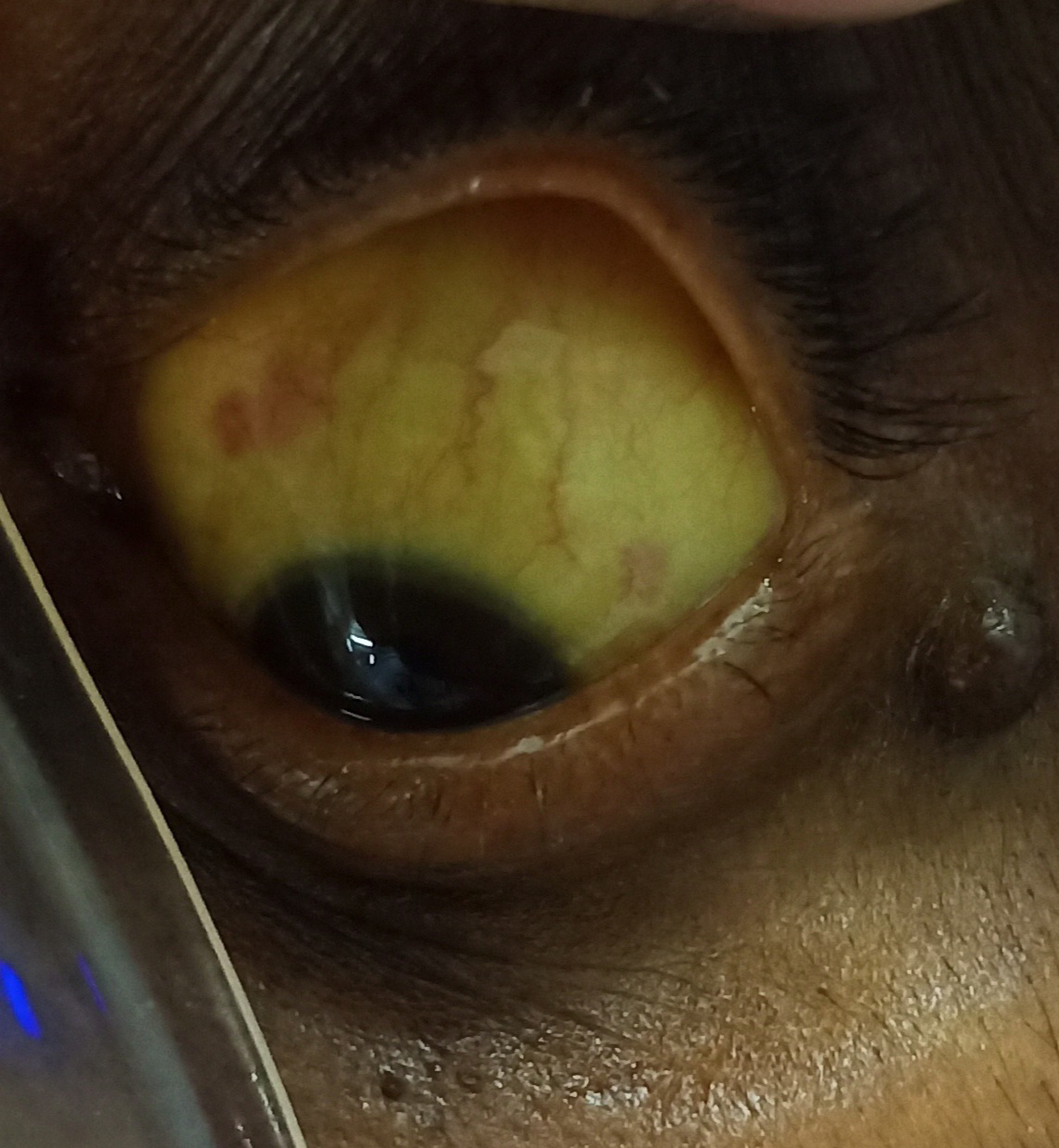
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box. 45 years old male pt came to opd with cheif complaints of shortness of breath (grade 2-3) since 20 days , complaints of loss of appetite since 20 days. Patient was apparently asymptomatic 35days back, then he developed shortness of breath for which he went to a local hospital after further investigation he was diagnosed with chronic kidney disease and underwent 4 sessions of dialysis.Then referred I/V/O dialysis. He was diagnosed with hypertension 1 month back and is on regular medi...